Do more with your donation
Automated Blood Donation is a unique donation process that efficiently and effectively separates blood components, allowing you to do more each time you donate.
EFFICIENT & EFFECTIVE
With Automated Blood Donation, less blood is removed per visit because only the needed components are used and the rest of the blood is infused back into the donor. This means that you can donate more, helping more people with each visit. Cascade Regional Blood Services and you, together, can ensure the needs of receiving patients in our community are met efficiently and effectively.
ARE YOU ELIGIBLE FOR AUTOMATED DONATION?
If you meet the criteria for donating whole blood and your platelet count is above a preset threshold, you are likely a good candidate for automated donation.

Blood Components
DOUBLE RED CELL
Double Red Cell donations allows you to give twice the red cells. Using the same apheresis technology, drawing red cells while the rest of your blood components are returned to your body. Red cells are the component most frequently transfused to patients at our local hospitals. Surgery patients, severe accident victims, cancer patients, and patients with anemia are common recipients of red cell transfusions.
Double red cells can be donated every 112 days. A double red cell donation takes about 1.5 hours.
Requirements:
• Men 5’1, at least 130lbs
• Women 5’5, at least 150lbs
• Preferred blood types, A-, O-, and O+
PLASMA
Plasma is the liquid portion of the blood that carries clotting factors and proteins. Plasma is collected through an automated process that separates plasma from other blood components, then safely and comfortably returns your red blood cells and platelets to you. Plasma is need to treat burn victims, trauma patients and those battling sever liver disease and cancer. If you are type AB you can make the most of your donation by becoming a plasma donor as patients of all blood types can safely receive AB plasma.
Plasma can be donated every 28 days and takes approximately an hour.
PLATELETS
Platelets are tiny cells in your blood that form clots and stop bleeding. During a platelet donation an apheresis machine collects your platelets along with some plasma, returning your red cells and most of the plasma back to you. A single donation of platelets can yield several transfusable units. Platelets are special because they are constantly needed by patients but they are hard to keep on our shelves because they have a short shelf life. Platelet donations last only 7 days. We rely heavily on frequent, regular platelet donors, just like patients rely on frequent, regular platelet transfusions. Platelets are most often used by cancer patients, burn victims, premature babies, organ transplant recipients, accident victims, and others facing life-threating illnesses and injuries.
A platelet donation can take between 80 minutes to 2 hours to complete. We understand this is a significant portion of your day, but we try to make the donation as easy as possible. We have portable video players, movies, and WiFi to keep you busy. You can donate platelets every 7 days, up to 24 times per year.
Join us! Please call an Automated Scheduler to learn more about automated donations.
What Happens to Automated Products after Donation
STEP ONE
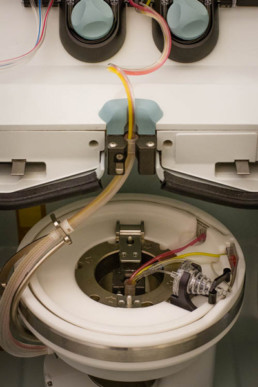
Automated donation by apheresis is the process of withdrawing whole blood and separating it into component parts (platelets, plasma or red blood cells) by spinning in a centrifuge. The needed components are kept and the rest is returned back to the donor.


STEP TWO
Platelets are stored at room temperature and placed on an agitator to keep the platelets from clumping together. They are also cultured to detect any bacterial growth and irradiated to inhibit the replication of white blood cells. Platelets have a shelf life of 5 days.
Plasma from automated donations is divided into individual units and frozen within 8 hours of collection to ≤ -18˚ C. Fresh Frozen Plasma, or FFP, can be stored for up to one year after collection. Plasma is couriered to the hospital in its frozen state and not thawed until just before transfusion.
Red cells from automation are already separated from plasma. An anticoagulant/preservative is added and it is filtered to minimize any remaining leukocytes (white blood cells) to prevent transfusion reactions. Red blood cells are refrigerated and have a shelf life of 42 days.

STEP THREE
As with whole blood donations, all automated donations are subjected to the same rigorous pre-donation screening and laboratory testing to ensure the blood’s safety. Please see our article, “What Happens to Blood After Donation” for a list of all laboratory tests performed on each donation.

STEP FOUR
After your blood donation has completed testing and been properly labeled, it is stored in large refrigerators and freezers at CRBS. It is now ready for distribution to hospitals.

STEP FIVE
The final step in your donated blood product’s journey is when a component from your donation reaches the right patient-typically within 10 days.
Products
RED BLOOD CELLS and WHOLE BLOOD
Red blood cells are the most common type of blood cell and carry oxygen from the lungs to all body tissues. Red Blood Cell transfusions are routinely used for surgical and trauma patients. Other patients who benefit from red blood cell transfusion include those with anemia and those with blood disorders such as Sickle Cell Disease.
Whole blood is most often separated into blood components but is used for infants on rare occasions as well as surgical and life support devices.
PLASMA
Plasma is the liquid portion of the blood in which the red cells, white cells, and plasma are suspended. It consists mostly of water containing proteins, electrolytes and nutrients. Plasma transfusion is used to control bleeding during surgeries and trauma, and to treat patients with clotting disorders and major burns.
PLATELETS
Platelets are tiny cells circulating in the blood. Platelets gather at a bleeding site and clump together to form a plug that begins to seal the blood vessel. They also release substances that promote further clotting. Platelets are often transfused to patients with bleeding disorders, and to those undergoing cancer treatments and organ transplants.
CRYOPRECIPITATE
Cryoprecipitate is a frozen blood product prepared from plasma. It is rich in clotting factors and commonly used to treat trauma victims and patients with bleeding disorders.
SPECIALIZED PRODUCTS
CRBS collects specialized blood products for use in research and patient care, such as autologous white blood cell products for manufacture (insert link to Dendreon? http://www.dendreon.com/). CRBS partners with MultiCare Health System to provide whole blood and platelets for pediatric heart surgeries though our Baby Blood Program. Special products are also collected for ECMO life support and LVAD placement surgeries. Over 170 such surgeries and procedures are conducted annually at MultiCare.
Services
THERAPEUTIC APHERESIS PROCEDURES
In addition to collecting blood to supply to our community hospitals, CRBS has a staff of highly-trained nurses who perform in-hospital procedures at MultiCare Tacoma General Hospital, MultiCare Good Samaritan Hospital and MultiCare Mary Bridge Children’s Hospital & Health Center. The procedures include:
- Red Blood Cell Exchange – The removal and replacement of a patient’s diseased red blood cells with healthy cells.
- Cellular Depletions – The removal of harmful amounts of platelets or white blood cells from a patient’s blood.
- Therapeutic Plasma Exchange – The removal and replacement of a patient’s plasma, in order to remove pathogenic substances or replace deficiencies.
THERAPEUTIC PHLEBOTOMY
Therapeutic phlebotomy is a blood draw procedure prescribed by a physician or other licensed health care provider. It is a treatment to reduce accumulation of excess iron in the body, resulting from conditions such as hemochromatosis and polycythemia. Therapeutic phlebotomy is done by appointment at our Tacoma, Puyallup, and Federal Way Donor Centers.